This report, co-published by Friends of the Global Fight, PATH, and JSI, identifies key lessons learned from the HIV response, offers future recommendations to help chart a way forward toward broader implementation of IPCC, and concludes with an action plan highlighting critical next steps that need to be taken to scale IPCC.
Person-Centered Care
What is Person-Centered Care?
Person-centered care does the following three things:
- Acknowledges people’s essential human dignity
- Treats people as individuals
- Seeks to understand what people value most about their treatment and care
At JSI, we put people at the center of health programs at all levels—individual, community, health facility, system, policy—because we know that each part of the health ecosystem contributes to person-centered care. We use behavioral science to understand people’s motivations and preferences and to learn what system and service delivery changes are needed to transform people’s experiences and improve health outcomes.
Person-centered systems and services provide many benefits:
- Improved access to care
- Increased health literacy
- Higher rates of client satisfaction
- Improved job satisfaction among the health workforce
- More efficient and cost-effective services
- Improved health outcomes

Resource Spotlights
Areas of Expertise
Our Framework
Our Person-Centered Care Framework uses a human-rights-based approach that focuses on the rights holder (person) and the obligations of duty bearers (e.g., providers, policymakers, caregivers). The five principles that surround the rights holder (at the center) establish a common vision for person-centered care. The principles can be operationalized and assessed at each socio-ecological level (i.e., policy and environment, health system, facility, community, and individual and family) through interventions within six domains, as labeled on the outside of the framework.
Measures of Person-Centered Care
Measurement is an essential tool for continuous quality improvement and accountability. That is why JSI developed a tool for HIV service providers to collaboratively measure person-centered care (PCC) at facilities providing HIV treatment, assess the facility’s ability to provide person-centered HIV treatment, demonstrate areas of strength for organizational learning, and tailor investments in further interventions or improvements.
Experience of Care
Experience of care encompasses all of the interactions patients and their families have throughout their health care journey. Studies show that quality of care and patient experiences will deeply impact health care utilization, outcomes, and behaviors. Improving experience of care relies on patient- or family-centered care, which respects and responds to individual preferences, needs, and values— placing the patient and family at the heart of decision-making.
Our Person-Centered Care in Action

In Ghana, JSI brings HIV treatment services closer to people by caring for them at multiple points of care (in facilities, communities, and homes based on each person’s needs and preferences). Our innovative approaches support adherence, overcome access challenges and build trust through providing home-based ART refills, and offering community- and facility-based services, or any combination in between.
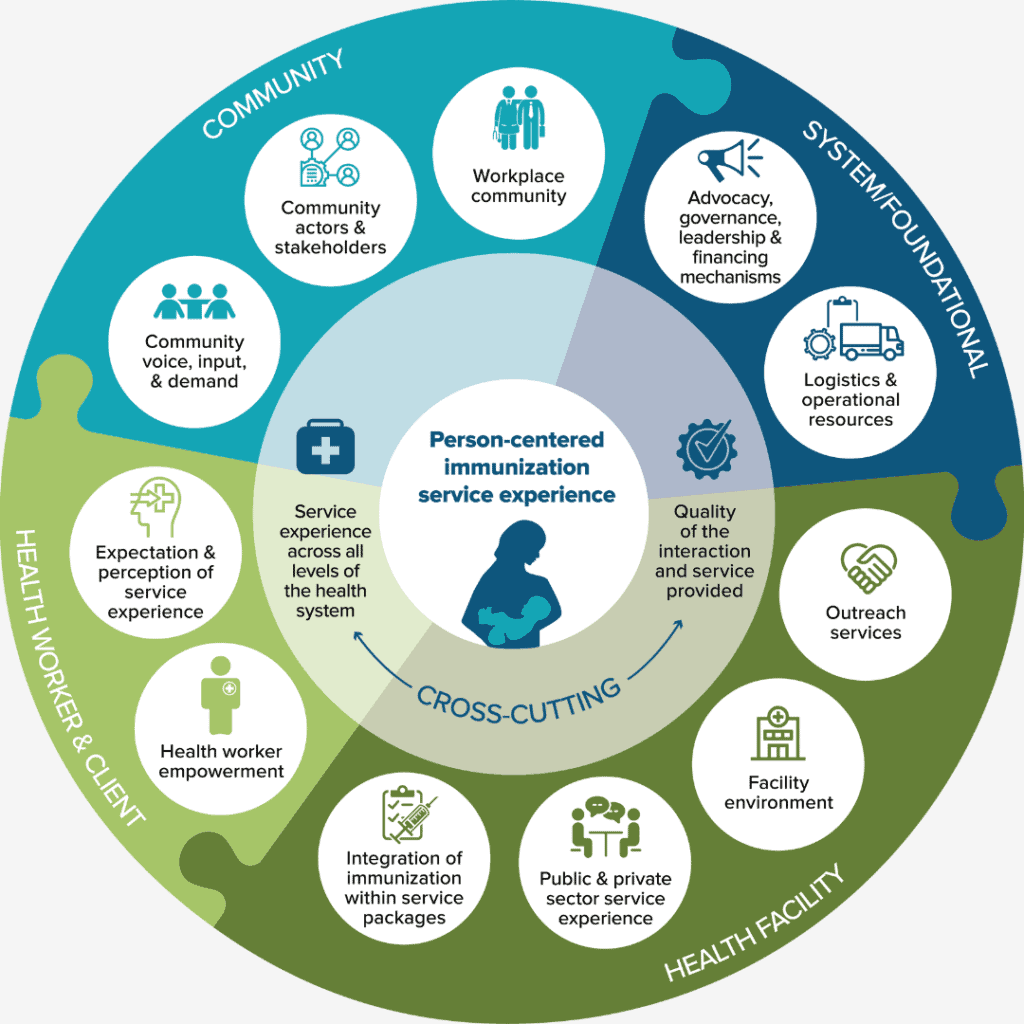
Immunization service experience plays an important role in ensuring that immunization programs are valued by and accessible to everyone. JSI designed an Immunization Service Experience (SE) Toolkit to introduce the concept of SE at country level for immunization staff and implementing partners. The five toolkit products are meant to spark discussion around how country immunization programs may address and improve the delivery and experience of immunization.

Through the Reproductive Health National Training Center (RHNTC), JSI trains and supports agencies that provide sexual and reproductive health services across the United States. The RHNTC provides online and in-person training on a broad range of topics to advance person-centered care. Examples of topics include improving patient experience, cultural humility and implicit bias, addressing weight stigma and bias, trauma-informed care, and providing affirming care to LGBTQ+ clients.
Related News and Stories
- Using Person-centered Care to Accelerate Progress toward the Sustainable Development Goals
- Accountability is Key to Delivering Person-centered Care
- Strengthening Immunization Services through Person-centered Care
- What Does it Take to Govern and Finance Person-centered Care?
- Advancing Person-Centered Maternal Care for Ethiopian Girls and Women
- New Year, Renewed Commitment: Making progress toward universal health coverage through person-centered care
- Person-Centered Care: Key Theme at 2022 International AIDS Conference
- Day of the Girl Child: Let’s Aim for A World Free of Cervical Cancer
- Happy World Contraception Day! Let’s Get to Work to Secure Girl’s and Women’s Reproductive Health Rights through Person-Centered Care
- Making Person-centered Mental Health Care a Reality
- How COVID-19 Facilitated Person-centered HIV Care in Zambia
- JSI Authors Outline Best Practices for Person-Centered HIV Care in Sub-Saharan Africa
- Beyond Theory Satellite Session
- Improving the Quality of Tuberculosis Care: Tools to Assess Quality of TB Services in High-Burden Countries
- Trust, Capacity, and Innovation Help Local Organizations Reach Last-Mile Communities
- Kyrgyz Nurses Provide Psychological Support and More for People with Tuberculosis
- New Journal Article Examines Human-Centered Design to Adapt Supply Chains and Digital Health Solutions in Kenya
- Educating Pregnant and Breastfeeding Mothers to Make Informed HIV Preventive Choices
- Contraceptive Method Introduction to Expand Choice
- Integrating Responsive Care and Early Learning with Nutrition Counseling Inspires Mothers in Ghana
- JSI Celebrates Helping Expand Access to Health Services for 17 Million Ethiopians
Partner with Us
We strive to build lasting relationships to produce better health outcomes for all.