This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognizing you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
In Nepal, nearly 1 in 30 children die before reaching their first birthday, with 66% of those deaths occurring in the first one month of life, the neonatal period. Almost half of all newborn deaths are due to neonatal infections, many of which can result from exposure of the newborn’s umbilical cord stump to pathogens through unhygienic delivery conditions or traditional practices.
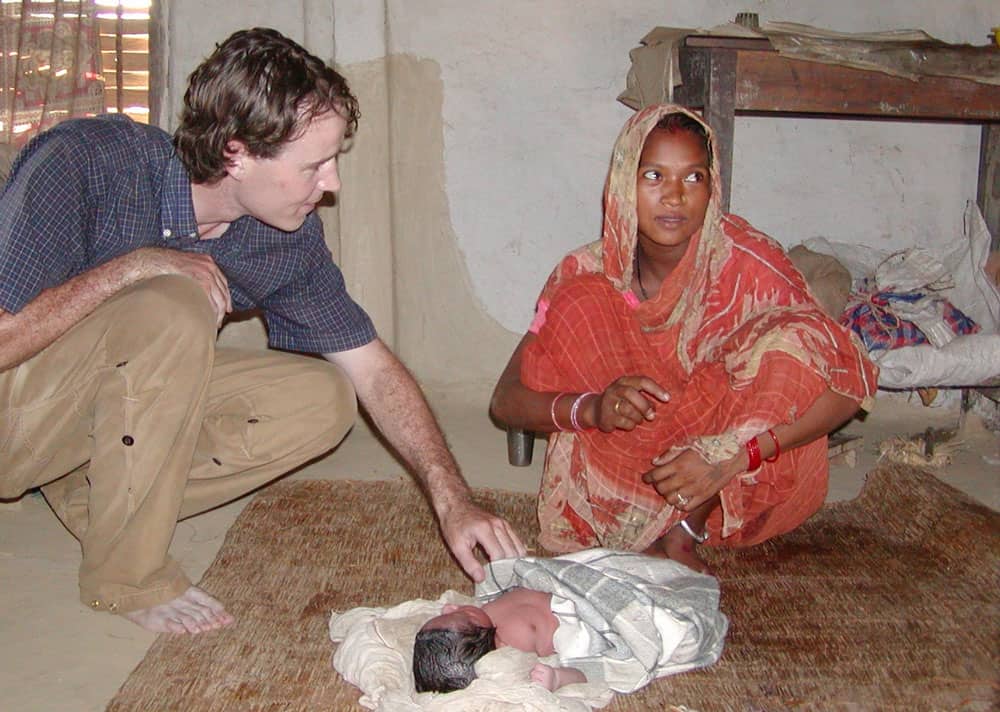
PHOTO CREDIT: LUKE MULLANY
In search of an innovation to save newborn lives, a group of researchers from the Nepal Nutrition Intervention Project-Sarlahi at Johns Hopkins University conducted a randomized controlled trial in the country from 2002–2006. They explored whether chlorhexidine, a safe and effective broad-spectrum antiseptic, could prevent neonatal infection and death when applied to a newborn’s umbilical stump after cord cutting.
Their study found that the use of chlorhexidine reduced neonatal mortality by 34 percent and prevented severe umbilical cord infection by 75 percent. Similar results from subsequent studies in Bangladesh and Pakistan further proved chlorhexidine’s potential as a lifesaving commodity.

With this evidence, the Government of Nepal convened a National Chlorhexidine Technical Working Group, comprised of representatives from the government, development partners, private pharmaceutical companies, and professional societies, to explore opportunities to implement chlorhexidine use for cord care.
In 2008, Lomus Pharmaceuticals, a Nepali company, created the first formulation of chlorhexidine gel in the world. Through a unique private-public partnership, the Technical Working Group oversaw two studies—one comparing the effectiveness of gel and liquid formulations and the other exploring community members’ preference for gel or liquid chlorhexidine. They found that the chlorhexidine gel was as effective as the liquid product and that community members preferred it more.
Having identified an acceptable and effective product, the Government of Nepal, with support from JSI and Plan Nepal, conducted a chlorhexidine pilot program in four districts from 2010–2011. The pilots showed that chlorhexidine could be scaled up with high coverage when integrated into ongoing government maternal and child health programs.
In 2011, the government approved the use of chlorhexidine for essential newborn care and committed to its nationwide scale up. To support the government in doing this, the JSI-led Chlorhexidine Navi Care Program (JSI/CNCP), funded by USAID through the Saving Lives at Birth initiative, was launched.

With support from JSI/CNCP and the country’s Ministry of Health, 15,437 health workers across all public health facilities and 2,860 health workers in 79 private health facilities were trained in chlorhexidine application. As a result, chlorhexidine is now regularly applied to infants born in these facilities.
Additionally, health workers counsel pregnant women about chlorhexidine use during antenatal care visits. While they encourage women to return to the hospital for delivery, they provide those who are in their eighth month of pregnancy with a tube of chlorhexidine and instructions on the proper application technique. This ensures that should the woman be unable to reach the hospital during delivery, she will still apply chlorhexidine to her newborn’s umbilical cord at birth.
To increase demand for chlorhexidine application and to reach all mothers with chlorhexidine gel, Nepal’s Chlorhexidine program trained 44,171 Female Community Health Volunteers (FCHVs) in chlorhexidine counseling and application. The FCHVs distribute chlorhexidine tubes to pregnant women and their families and provide instructions on how to use the gel correctly in the case of home delivery.
In order to raise awareness about chlorhexidine, JSI/CNCP carried out a nationwide mass media campaign. The project broadcast 5,321 television and 423,720 radio public service announcements and distributed 1,100,000 instructional aids. Nepal’s 2016 Demographic Health Survey found that chlorhexidine was the most frequently seen and heard health message in the country, reaching 45 percent of women and 46 percent of men.
JSI/CNCP also conducted targeted social and behavior change programming to reach communities with limited access to media and health services. Community mobilization, street dramas, wall paintings, and other local approaches were used to ensure that hard-to-reach communities were aware of, and had access to, chlorhexidine.
A television commercial that aired in Nepal promoting the use of chlorhexidine.
In 2015, a powerful earthquake struck Nepal damaging many health facilities and hampering delivery conditions. This prompted the government to rapidly scale up chlorhexidine implementation through earthquake response efforts to protect newborn health.
Out of the 14 earthquake-affected districts, five had already introduced chlorhexidine so JSI/CNCP rapidly implemented the chlorhexidine program in the remaining nine. Chlorhexidine was also included in the reproductive health kits that were distributed in the 14 districts.
Nepal, the first country to introduce and scale up chlorhexidine for newborn cord care, has become a “living university” for the world. Through the JSI/CNCP project, it has hosted over 200 visitors from 20 countries that are seeking to scale up chlorhexidine use. To bring this lifesaving intervention to newborns around the world, JSI has provided short-term technical assistance to other countries including Bangladesh, Ethiopia, Liberia, Madagascar, Mozambique, Niger, Nigeria, and Pakistan, sharing lessons learned from the program in Nepal.
As of November 2017, chlorhexidine had been applied to the umbilical cords of 2.1 million newborns in Nepal, resulting in an estimated 9,600 lives saved. The program has been rolled out in all districts in the country and the government has committed to continue strengthening it to reach all newborns.
Today, chlorhexidine has been fully integrated into the government health system. It is a key component of essential newborn care and has been included in government health training curricula and policies. Chlorhexidine has also been incorporated into the Health and Logistics Management Information Systems as well as periodic surveys that regularly provide information on product availability and use to strengthen implementation.
Outside of the public health system, it is estimated that more than 4,122 private health facilities and 44,000 FCHVs are providing chlorhexidine services. Additional training in private facilities is ongoing to reach all institutional births with chlorhexidine.
With support from JSI/CNCP and partners, the Government of Nepal developed processes to ensure uninterrupted chlorhexidine supply and began procuring and supplying chlorhexidine in 2016. Although JSI/CNCP’s support to the program ended in December 2017, the government has committed to continue implementing and improving the program as part of its efforts to save newborn lives. The Director General of the Ministry of Health affirmed this by saying, “We take responsibility to ensure the availability of chlorhexidine for every child.”

At the JSI/CNCP closeout event, USAID/Nepal Mission Director Peter Malnak said, “The story of chlorhexidine in Nepal shows that a small idea, coupled with cross-sector partnership and strong government leadership, can successfully reach national scale and impact millions of lives.”
JSI/CNCP’s chlorhexidine scale-up experience in Nepal shows that this intervention can be integrated successfully into the health system. The lessons learned are—and will continue—informing health programs around the world seeking to scale up lifesaving innovations.
Get more information and resources from the JSI/Chlorhexidine Navi Care Program.