The Power of Partnerships for Improved Routine Immunization in Nigeria
April 25th, 2019 | viewpoint
In Nigeria, routine immunization (RI) programs have faced myriad challenges. A lack of awareness, trust, and trained health workers – particularly in hard-to-reach and rural areas – as well as poor-quality health information and service delivery issues have resulted in some of the lowest coverage rates in the world.
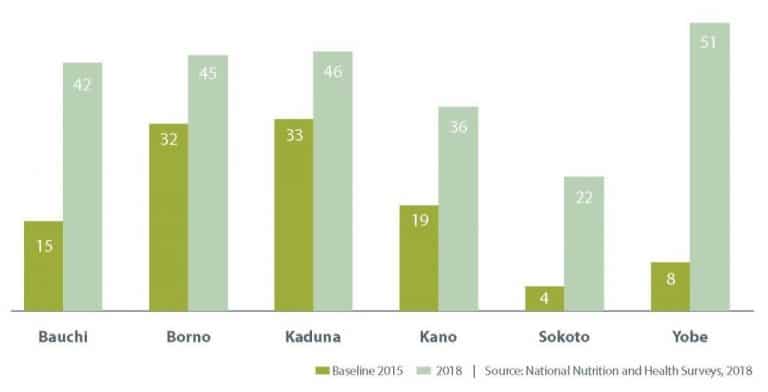
Coverage rates across regions also vary, with the country’s lowest rates in the northern states of Bauchi and Sokoto. The 2018 National Nutrition and Health Survey revealed that only 42% (Bauchi) and 22% (Sokoto) of children in these states received the third dose of pentavalent vaccine by their first birthday.
To address these challenges, the Maternal and Child Survival Program (MCSP) supported an innovative, multi-partner approach in the region, providing technical assistance for implementing memorandums of understanding (MOUs) dedicated to improving both states’ RI systems. The MOUs between the Bauchi and Sokoto state governments, USAID, and two foundations — the Bill & Melinda Gates Foundation (BMGF) and the Aliko Dangote Foundation (ADF) — were two of six MOUs related to RI that were implemented across northern Nigeria.

How were the MOUs funded?
Under the MOUs, the Bauchi and Sokoto state governments and ADF and BMGF contributed “basket funds” into dedicated state-managed program accounts. The MOUs were designed to move the RI programs toward sustainability through a phased funding approach that committed ADF and BMGF to provide 70% of funds for RI programming in the first year, while the states provided 30%. In the second year, the foundations and the state governments shared funding at 50% each. In the third year, the foundations provided 30% of funds and the states 70%. USAID provided technical support through MCSP.
What were the MOU results?
In Bauchi, RI coverage for the third dose of pentavalent vaccine nearly tripled, from 15% at baseline in 2015 to 42% in 2018. In Sokoto, the third dose of pentavalent coverage increased fivefold, from 4% in 2015 to 22% in 2018. (The four other states implementing RI MOUs showed similar increases in pentavalent coverage.) For core service delivery indicators, the MOUs in Bauchi and Sokoto states also documented increases in fixed and outreach services and numbers of health facilities providing RI services.
How did the MOUs work?
Our experience providing technical assistance to the Bauchi and Sokoto MOUs – as well as the experience of the six MOUs at large – is a source of lessons learned and a recommended process for developing and implementing an MOU for improving RI systems. The process followed four stages: (1)design; (2) start-up; (3) implementation; and (4) transition.

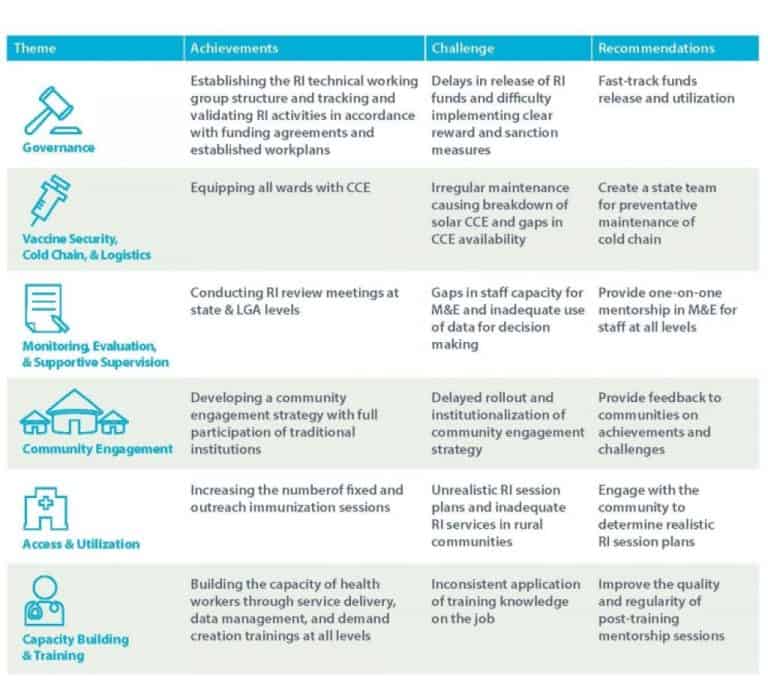
Design: During the design stage, the MOU partners engaged with stakeholders, conducted an assessment of RI program needs, and developed a clear rationale for the MOU partnership and goals across six RI thematic areas:
Start-up: During the start-up stage, the partners developed a strategy to achieve the established goals and address operational components, including funding requirements, funding sources, and a harmonized workplan that aligned all government and partner activities in one document. The harmonized workplan allowed only activities in the workplan to be implemented; an activity not in the workplan had to be approved by the MOU partners and added to the plan before it could be implemented.
Implementation: In the implementation stage, MOU stakeholders established a working group (WG) structure to facilitate coordination and communication. Under this structure, the RI WG Chair was responsible for coordinating decision-making and daily RI program operations. Sub-WGs were established under the overarching RI WG to address specific needs across the six RI thematic areas.
Transition: The transition stage saw the phase out of donor funding and plans developed for ongoing programmatic, financial, and political support to ensure the continuity of strengthened and sustained RI systems. In Bauchi, the transition extended the MOU into a fourth year with the state government assuming 100% of the funding, while the MOU in Sokoto was extended for an additional five years with the foundations continuing to provide 30% of the funding.
To learn more, download this poster illustrating the background, methods and key conclusions of this work. Case studies from Bauchi and Sokoto states are also available.
More detailed presentations of the MOU process and its stages – as well as lessons learned and recommendations – will be available in a forthcoming MCSP document, “Implementing an MOU with Basket Funding to Improve RI Systems: A Start-up Guide Compendium.”
Originally posted by MCSP on April 25, 2019.
Written by: Leanne Dougherty, Folake Olayinka, and Kate Howell
We strive to build lasting relationships to produce better health outcomes for all.