This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognizing you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
We may have made progress in longevity, but the benefits aren’t distributed evenly.
The 20th century ushered in remarkable increases in life expectancy in the United States. These gains have been realized in some form by all races and genders, but they are not distributed equally across racial/ethnic subgroups.
Public health efforts led the advances by reducing infant and child mortality in the first half of the century, while medical advances added a smaller but significant number of years to adulthood in the latter half. In 1900, average life expectancy in the U.S. was only 47.3 years; by the end of the century, it had risen to 76.8—an extraordinary achievement in 100 years.
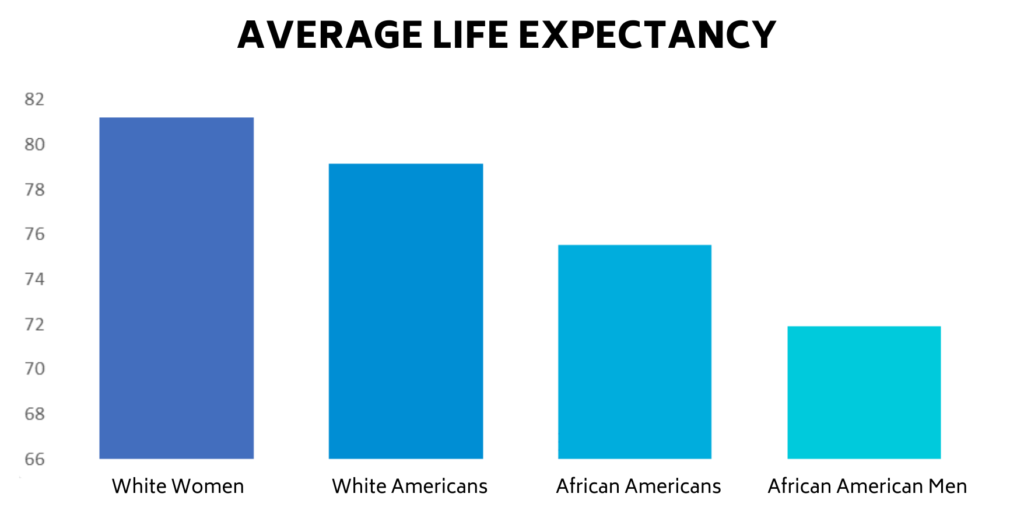
Advances of the 21st century have continued to add incremental gains to the second half of life. However, when you dig deeper, significant racial disparities appear. While white Americans have an average life expectancy of 79.12 years, African Americans have an average life expectancy of 75.54. The greatest contrast is seen when considering race and gender. The average life expectancy of a white female in the U.S. is currently 81.2 years, while the average life expectancy of an African American male is only 71.9, nearly a 10-year difference. Some of the discrepancy can be attributed to premature death of U.S. males in adolescence and early adulthood. But that is not the whole story.
If you focus on what demographers refer to as “survivorship”—the likelihood of surviving from young adulthood to older adulthood—the differences become stark.
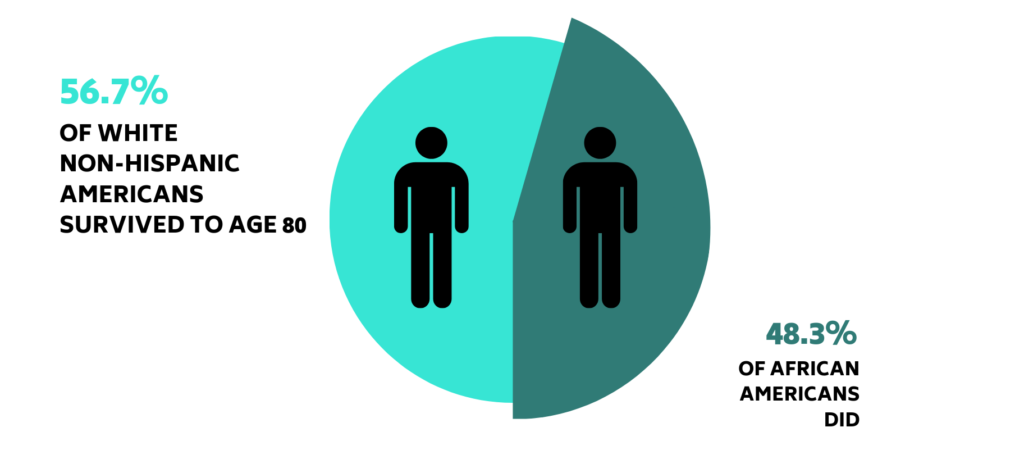
U.S. data from 2017 show that 57.6% of white, non-Hispanic Americans survived to age 80, while only 48.3% of African Americans did.
The reasons for these differences are now receiving considerable attention. Once attributed to behavioral risk factors, it has become clear that behavior alone does not account for the racial longevity gap. White Americans, for example, have far higher rates of smoking, heart disease, and lung cancer than African Americans, yet they live longer on average. Research is beginning to demonstrate that a host of social and economic factors contribute to health outcomes and longevity.
Structural disadvantages of past decades have limited African Americans’ access to healthy food, a safe environment, public transportation, physical activity, good education, and a livable wage. These factors create and compound health risks over time. There is emerging evidence that racism creates systemic stressors that lead to poor health outcomes and accelerate aging. Researchers refer to this as “biological weathering” and can demonstrate the shortening of telomeres—evidence of early aging—in people who are exposed to cumulative stress.
In addition to shortening lifespan, these differences often result in a decline in functional ability that causes economic problems and creates caregiver burdens as people age. Economic insecurity is particularly pronounced in older women of color. A 2013 study found that African American single women between 65 and 84 held a median wealth of only $55,700, compared to a median wealth of $187,000 in their white non-Hispanic counterparts. Limitations in financial assets reduce choices for housing, food, and social interaction. These factors negatively affect mental health and cognitive ability. In later life, the interplay of limited economic and social options have a cascading effect that results in isolation and disability.
As we celebrate the achievements our nation has made in longevity, it is critical that we recognize that millions of us are not fully benefiting from them. Policies and programs to close these gaps and direct resources toward them will help us eliminate racial longevity disparities.
Written by Margaret Franckhauser, U.S. Director of Aging