All for One and One for All? The Immunization and COVID-19 Vaccination Dilemma
April 26th, 2021 | viewpoint
Terms like ‘equity’ and ‘country-led’ are used regularly for the COVID-19 vaccination roll-out processes, but what is happening on the ground, particularly in lower and middle-income countries? COVAX, the vaccines pillar of the Access to COVID-19 Tools (ACT) Accelerator, was conceptualized as an ‘all for one’ approach to align manufacturers, supply, and demand – and foster equitable access to COVID-19 vaccines. Despite its remarkable success, COVAX has limitations due to overburdened national health systems, parallel vaccine procurements, and constraints in supply and operational funding in many countries. This impedes the ability for COVAX to be ‘one for all’.
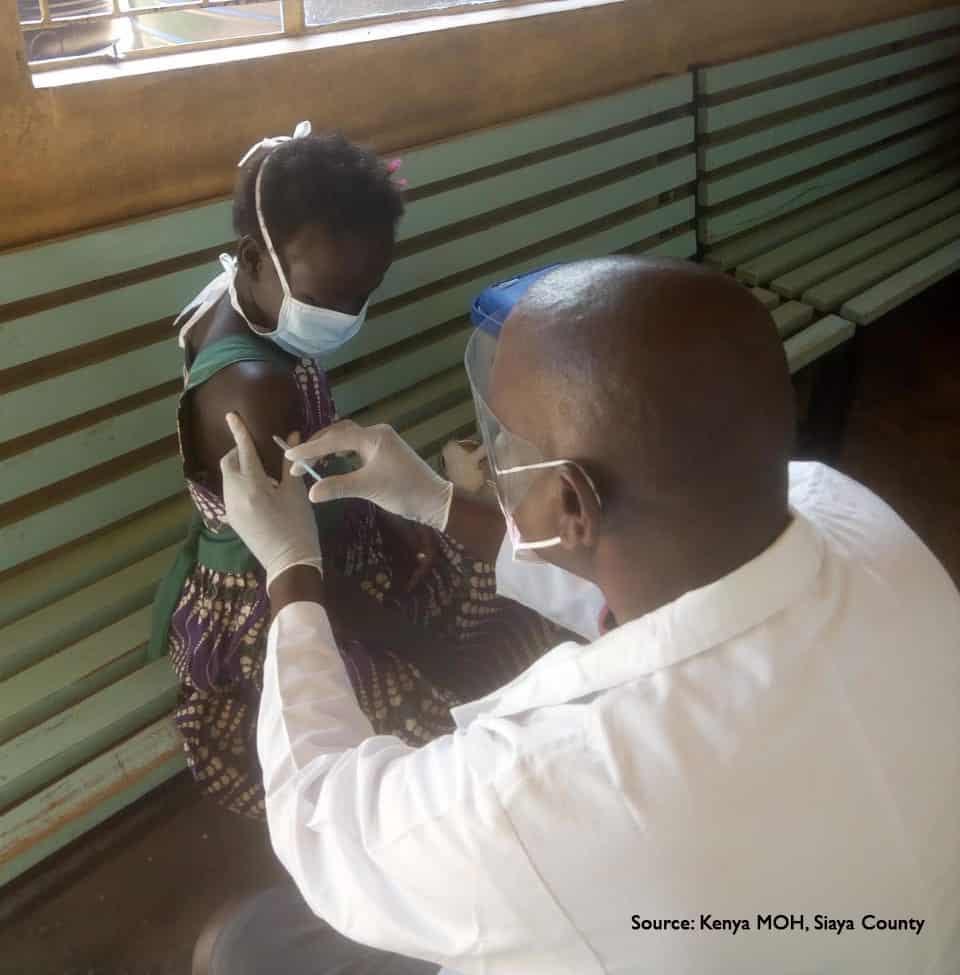
In the past six months, COVID-19 vaccines have been introduced in a pressure cooker. The usual processes for new vaccine introduction have been compressed into a short time, using systems that have not been developed or sufficiently modernized for this task and amplifying coordination challenges.
In March/April 2020, we were sounding the alarm on the need for intensive preparations for the eventual COVID-19 vaccine roll-out, given our experience with new vaccine introductions and outbreak response. We’ve all been hearing daily about how many people have been vaccinated in our own countries and around the world — and the inequities.
International coordination takes dedicated and sustained efforts with multisector experts. Globally, we were not prepared for this pandemic. Immunization systems, although well-established across the world, are complex. Few countries are set up to efficiently provide vaccines to adults and adolescents(for decades the primary focus of routine immunization programs has been on ensuring that children, age 0-24 months, are immunized. Recent country learning on nationwide HPV vaccination, for example, has shown the need for long-term models and strategies to engage with other sectors and departments, like education and cancer prevention). Life-course vaccination is a priority within the Immunization Agenda 2030 (IA2030) and now has increased urgency given COVID-19.
In the past six months, gaps in the vaccine delivery and immunization systems for COVID-19 vaccination have become clearer, from the point of manufacture (can they produce enough to meet extreme demand?), to supply chains (are the vaccines arriving, stored, and distributed efficiently?), point of administration (are enough health care workers trained to deliver the vaccine to meet the need with sufficient session sites?) to acceptability and uptake (are people, particularly the most vulnerable groups, confident and able to be vaccinated?). And if people want more information (not necessarily hesitant, which can be a misleading and blame-laden interpretation), how do we best reach them?
Despite the increasing and valiant vaccination efforts (with particular recognition of our extremely dedicated and overburdened health workers around the world), COVID-19 continues to percolate and affect more people. As we prepare for at least another year with this pandemic, we need to take a step back and examine what needs to be done differently to adapt systems for efficiency and equity.
How do we move forward to meet the world’s vaccination needs, for COVID-19 and more broadly?
A seismic shift needs to happen among donors and implementing partners to more effectively listen, seek inputs, engage, and resource civil society, iNGOs, and local health groups and organizations to help them solve issues in their countries and communities.
USAID, the Bill and Melinda Gates Foundation, and other funders have supported more local engagement, but program design and decision-making are still largely driven by external donor agencies—with their inherent processes that are ill-equipped to respond quickly in a pandemic. Civil society, along with Ministries of Health, must be resourced to steer and manage preventive health solutions. To reach priority populations (like elderly) and to ensure equity with COVID-19 vaccines, cross-sector units, such as infectious disease agencies, the private sector, and groups that serve high risk adult and aging populations must be proactively and sustainably part of the COVID-19 pandemic planning and response. This is particularly urgent for COVID-19 vaccination.
Preventive health services have received insufficient support for decades, particularly for ‘routine’ adolescent and adult public health programs like immunization. Few platforms are in place in countries to assist with HPV vaccination, for example (e.g., robust school health programs) or, as we are currently seeing worldwide, for adult vaccination against COVID-19. Public sector primary health care services are often disproportionately focused on curative care. Some private sector insurance programs offer preventive health services, but often people have to pay for them. COVID-19 vaccination may cost people in some countries.
Finding where adults live and receive their health services is not easy. Rural and remote communities need tailored strategies to reach them (particularly if outreach services are sporadic or if a vaccine requires an ultra cold chain). Urban dwellers move about, use different health facilities, and may be difficult to find. Working with civil society organizations and the public and private sector across health program areas (HIV, diabetes, etc.) will be critical to success, as we have seen in our urban immunization analysis and work across several countries, including Democratic Republic of the Congo and Haiti.
This is the elephant in the room. Funders often resource easier-to-measure activities and commodities: number of vaccines ordered; number of vaccines administered; equipment procured and distributed. But the day-to-day costs of health operations are overwhelming for most countries. From health worker salaries and contracts to training and monitoring vaccination roll-out and uptake, the costs of introducing a new vaccine are significant — and must be continued for onward years. Other examples include expenses for service delivery (such as travel and staff and community support to reach remote or urban poor communities), continuous communications for maintaining and increasing demand and confidence, and updating reporting and tracking systems (for the vaccines and syringes as well as individuals who have been vaccinated and who still need to be vaccinated). These operating costs must be adequately budgeted and resourced annually and recurrently, not just in spurts during emergencies or campaigns.

The ‘new’ challenge with COVID-19 vaccines is that they are being introduced in all countries within a period of just a few months. Other new vaccines have been phased with countries over several years (based on the countries’ longer-term vaccine introduction prioritization and preparatory processes). Additional operational resources specifically for COVID-19 vaccination are therefore needed for at least the next 2-3 years.
With every aspect of COVID-19, not only is the pressure cooker on high but there are also many ‘Executive Chefs’ in the kitchen and proposed new technologies. There are not enough ‘line cooks’ or other immunization experts who know on-ground preventive health and are sufficiently resourced long-term to ensure harmonious and practical delivery of immunization services. If funders, national public health systems, CSOs, communities, and implementing partners can adapt the lessons learned thus far in the COVID-19 pandemic to adjust the menu of solutions and resourcing models, we can better move forward as ‘all for one’.
Written by Lora Shimp
We strive to build lasting relationships to produce better health outcomes for all.