Improving Community Outcomes through Health Center Program Data [Part 4]
August 18th, 2020 | story
In the fourth and final of our UDS series, learn how the universal data system improves clinical performance for community health centers.
As the healthcare landscape changes with a greater understanding of how to provide care and adjustments in financing, the UDS evolves to meet the needs of target populations and communities.
The UDS is increasingly focused on clinical care within the health centers, and assuring that any disparities in performance and outcomes are addressed. Health centers now report a number of metrics that show the effectiveness of initiatives in addressing specific health concerns such as diabetes, hypertension, and opioid misuse.
“We can see what’s happening at the community level and what’s making a difference,” Lewis said. “For instance, we have ways to measure the impact that health centers are having on managing various diseases, and then we can look at what they’re doing that makes a difference.”
Administrators have put extensive effort into incorporating clinical performance measures aligned with national standards to assure that patients are receiving the highest quality of care and that the organizations are prepared for coming changes in the way health care is paid for based on clinical results.
Based on the clinical measure reported data and use of electronic health records to support reporting, HRSA has also been able to provide performance incentives, quality improvement awards that are based on such things as the use of electronic health records and progress on certain clinical measures.
Health centers also get help from the HRSA Health Information, Technology, Evaluation, and Quality Center on improving their electronic health record systems. The center, which JSI operates in partnership with Westat, supports health centers in using electronic health records and collecting accurate clinical data that can be used to improve clinical outcomes. The center identifies and disseminates promising practices and resources for using health information technology.
Integrating the electronic health records with the UDS has helped to improve the accuracy and efficiency of reporting. It has also helped to bolster efforts to use the UDS to identify opportunities that benefit patients.
Moving forward as measures are refined and added, there will be even more opportunities to use the UDS to understand how care is being delivered, Lewis said.
“It is significant that the UDS is standardized to provide the same types of data collected in the same format from health centers all over the country. That permits you to make accurate, relevant comparisons,” Lewis explained. “There is so much value in having this foundation of 20 years worth of high quality, reliable data,” she said. “This is something that centers, researchers, and others can use to really demonstrate how care can be effectively provided while creating new opportunities.”
As the program continues to grow, there are typically more applications for funding of new and expanded locations and services than there are funds to support them. Existing health centers have overlapping service areas, with some communities served by many organizations, but where additional needs remain unmet. One of the biggest challenges for HRSA and for entities in the community, is determining where the greatest needs are and tying these to the proper resources.
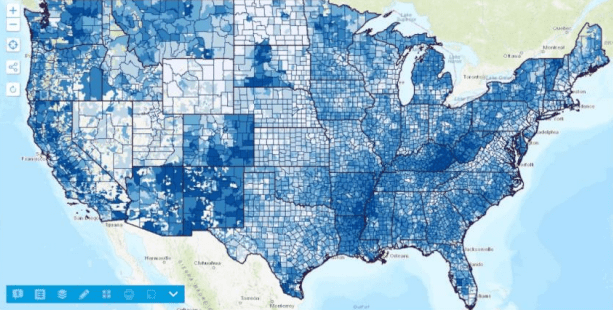
Here again, we created a new analytic approach to the UDS data that is collected, developing a highly targeted resource for use within HRSA, and externally by the existing health centers and others seeking new funding. The “Service Area Analysis” tool – shared externally on the web as the UDS Mapper – is a GIS-based platform which provides a wealth of information about the role of the health center program, and individual organizations, based on the ZIP code of patients seen each year. .
Adding the collection of patient ZIP code by insurance to the reporting requirements made it possible to track more accurately where patients were coming from, to aggregate the information across all health centers, and to connect that data to population-level statistics from the Census’ American Community Survey.
It’s now possible to see, on an interactive map, such things as the percent of different target populations served (total, low income, Medicaid, etc.), the trend in health center utilization across years, the quantity and portion of target populations not served, and the relationship between the service locations and the community utilization. Unmet needs can be visualized and the impact of adding or changing resources can be readily assessed.
 The UDS Mapper is open to anyone who registers online (through a collaboration with HealthLandscape) but target users are staff from current and prospective health centers, HRSA project officers, Primary Care Associations, State Primary Care Offices, and community planners. Use of the tool and the underlying data has been formally incorporated into the grant application process, and JSI uses the back-end data to conduct analyses supporting the grant review process.
The UDS Mapper is open to anyone who registers online (through a collaboration with HealthLandscape) but target users are staff from current and prospective health centers, HRSA project officers, Primary Care Associations, State Primary Care Offices, and community planners. Use of the tool and the underlying data has been formally incorporated into the grant application process, and JSI uses the back-end data to conduct analyses supporting the grant review process.
“It’s really a powerful tool that gets into the important nuances of need,” Turer explained
There might be five health centers in one city, but the map will indicate if there is a need for even more.
It can also be used to track and highlight areas of concern such as changes in insurance – an area of key importance after the passage of the Affordable Care Act and the ongoing transition to Medicaid expansion by states..
“It allows people to ask better questions about what is going on across the country. You see these shifts happening and that opens up opportunities to investigate the reasons behind them. Then you can make determinations about how best to address them,” Turer said.
Improving Community Outcomes through Health Center Program Data [Part 3]
The Rise of the National Health Centers [Part 2]
Using Data to Reduce Barriers to Colon Cancer Screening [Part 1]
We strive to build lasting relationships to produce better health outcomes for all.