Telehealth: Yesterday, Today and Tomorrow
March 15th, 2021 | story
In 2020, the Pueblo Community Health Center (PCHC) served a little over 27,000 people. Its patient base is primarily people who live at 200% of poverty and below, and about two-thirds of all patients identify as Hispanic, Latino, Latina, or Latinx.
PCHC has a large perinatal program, but like most community health centers, it is focused on serving people of all ages who have a variety of primary care needs, from acute urgent to preventive care to chronic disease management. PCHC offers behavioral health, oral health, and a variety of enabling and supportive services.
Prior to the COVID-19 pandemic, telehealth was not among PCHS’s service options; there wasn’t patient demand and telehealth programs were not reimbursed by the health center’s payers.
In an ideal situation, PCHC would have surveyed patients and providers before initiating an expansive telehealth program, but in 2020, the pandemic thrust PCHC into telehealth to assure its patients would be served.
Telehealth started in earnest at the end of March. In May, PCHC staff surveyed a sample of patients who were seen during the first 30 days of telehealth. They learned that 86% were comfortable with virtual care, most of which were over the phone. The survey also indicated that:
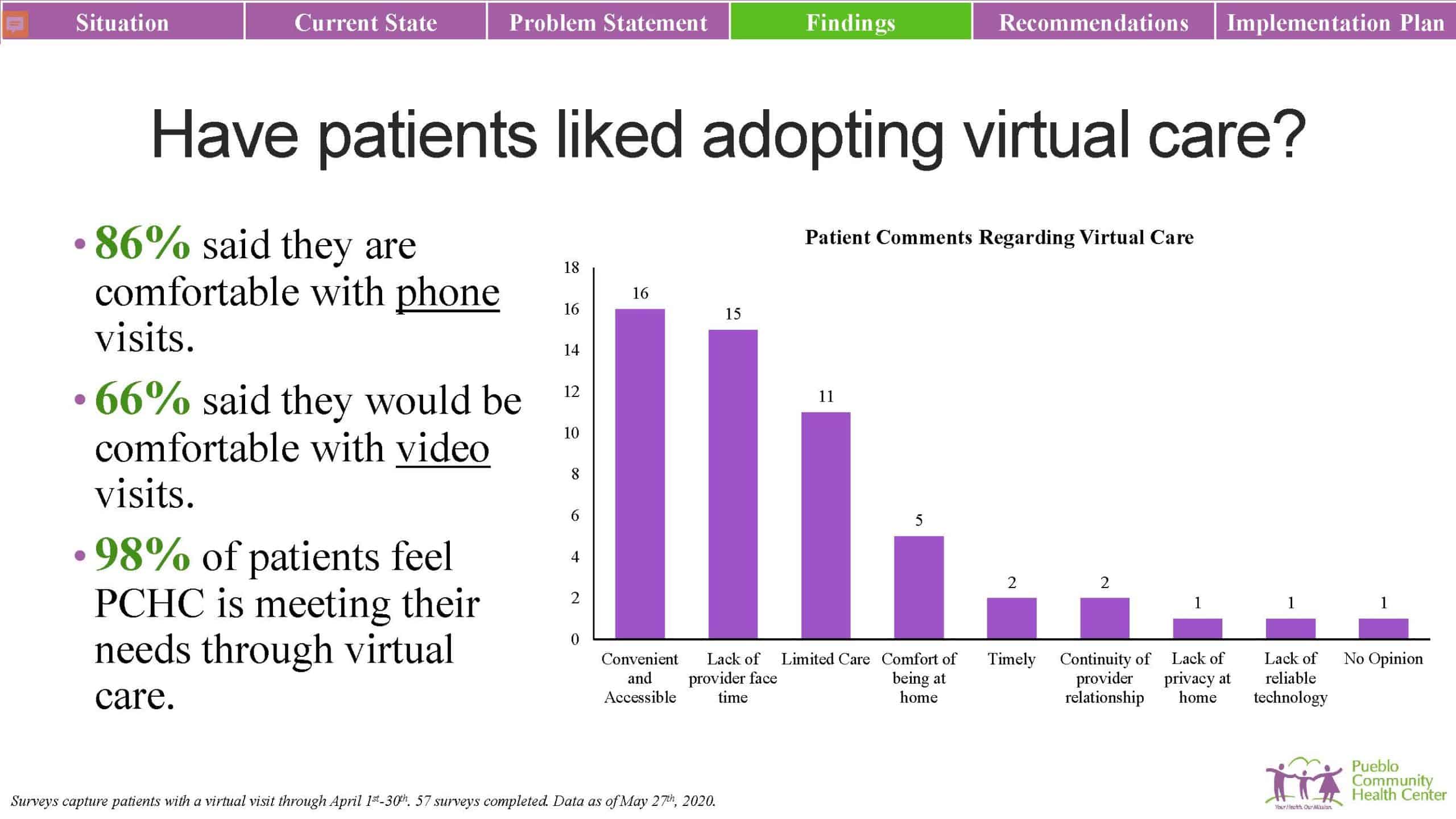
Patients clearly valued in-person, face-to-face contact. In the summer of 2020, PCHC adjusted provider schedules to accommodate more in-person visits and the health center became more proficient with COVID-19 transmission control within their facilities. However, as of the end of 2020, PCHC has maintained at least 50% virtual care.
The survey indicated providers’ comfort with telehealth, including which services they were confident and proficient providing virtually and those they found challenging. Providers were comfortable using telehealth for chronic care management, routine follow-up appointments, medication management and check-in with patients, as well as mental health and simple acute visits that don’t require hands-on physical examinations.
Care that is challenging to deliver virtually includes pediatrics, rashes and lesions, and anything that requires a physical examination. And of course vaccines, immunizations, annual wellness exams, and anything severe (e.g., a constellation of conditions that require an in-depth interview and physical examination). The literature supports what PCHC heard from patients and providers: telehealth is suitable for chronic care management, medication management, and behavioral health care. It is less suitable for patients who have multiple complications, prenatal care, and conditions that require hands-on care. Regrettably, preventive care also has extreme limitations.
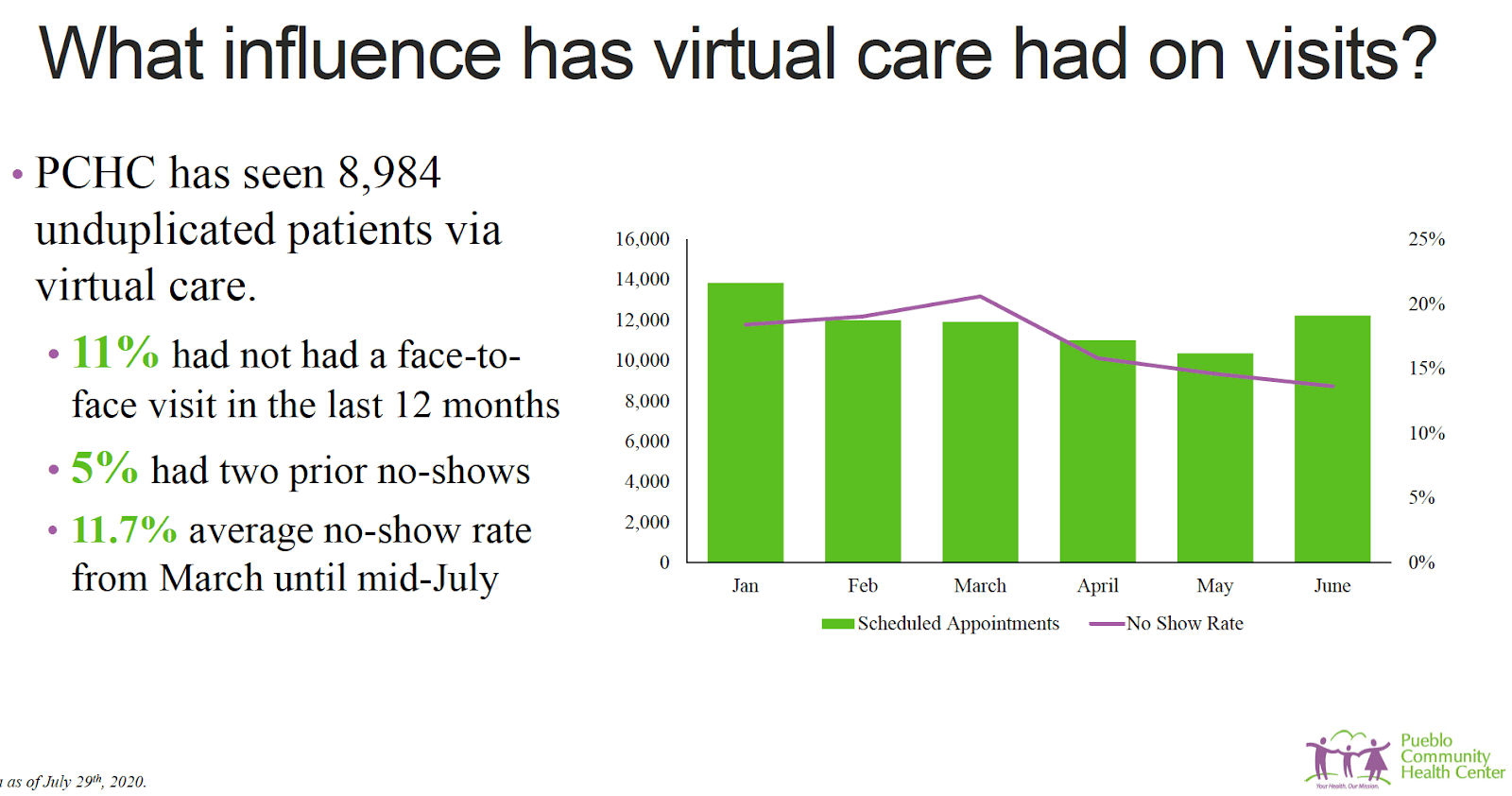
Virtual care has reduced some barriers for patients at PCHC and because of that they attend their appointments more consistently. From the onset of the pandemic through mid-July, the no-show rate was below 12%; before the pandemic, it was routinely 17%, 18%, 19%, even 20%. It became clear that telehealth can help patients achieve better health status.
In early April, hypertension was the number one diagnosis, aligning with what the providers were comfortable delivering virtually. Long-term use of oral hypoglycemic drugs (medication management for a diabetic patient) and management of type 2 diabetes were high-frequency codes showing up in telehealth. They matched the pre-pandemic, non-telehealth rates, and aligned with what the literature said patients were comfortable receiving over telehealth and what providers could deliver confidently and in accordance with the care standards in which they take pride.
Eighty percent of telehealth at PCHC is telephone-based encounters, to which patients adapted easily and which work well in its team-based care model. But video interactions are more robust and akin to in-person visits than telephonic interactions, and the health center is working to increase video modality access. Furthermore, payers such as Medicare reimburse differently for phone than video, and other payers may follow suit.
From the onset of the pandemic, PCHC functioned at 50–60% capacity, but has recently attained pre-pandemic levels of service. Levels of mental health care have exceeded pre-COVID rates, and there are fewer missed appointments. And for people—such as those with anxiety—who are less comfortable being served in person, virtual care offers a secondary advantage.
———————–
At the end of 2020, Senior Consultant, Stacey Moody, connected with our longtime partner Donald Moore, chief executive officer of the Pueblo Community Health Center (PCHC) in Colorado. Donald told us how PCHC implemented telehealth throughout the pandemic while aiming to maintain its ideal care model.
Listen to the full conversation on our podcast.
https://soundcloud.com/jsihealth/telehealth-a-tool-to-support-your-integrated-care-approach
We strive to build lasting relationships to produce better health outcomes for all.